WHAT IS PSORIATIC ARTHRITIS (PsA)?1,2
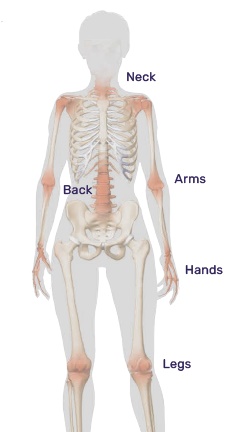
PsA is a type of arthritis that causes joint pain, swelling, and stiffness that usually occurs in combination with a chronic skin condition called psoriasis. Psoriasis presents as patches of irritated, inflamed red skin that are often covered with white scales.